Intrahemispheric symmetry of brain perfusion. Part 3. Assessment of neuropsycological state of patients based on SPECT data
DOI:
https://doi.org/10.3103/S0735272722080015Abstract
The third part of a series of papers deals with the diagnostics and treatment of patients, both military personnel and civilians, who have suffered traumatic brain injury (TBI) and barotrauma due to combat concussion (CC) with the development of post trauma stress disorder (PTSD). The main method for diagnosing neuro-cognitive changes in such patients is neuropsychological testing (NPT). However, based on different types of questionnaires, the NPT results can have significant inaccuracies associated not only with the subjective opinion of doctor, but also with inadequacy, and, sometimes, with deliberate actions of patients. This leads to the need of developing new objective diagnostic techniques that would confirm and refine the NPT results.
The current paper presents the development of the methodology for assessing the neuropsychological state of servicemen with CC-caused mild TBI based on single-photon emission computed tomography (SPECT) data, in particular, based on the analysis of volumetric cerebral blood flow (CBF) and perfusion intrahemispheric symmetry (IHS) in segments of the brain.
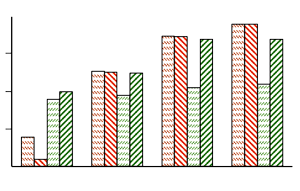
The data of 31 patients with moderate TBI due to CC were analyzed. The consequences of TBI should be considered remote, since at the time of their comprehensive examination from 6 to 12 months passed after the contusion. NPT was used to assess the degree of vegetative disorders according to Wayne of psycho-emotional sphere, the severity of symptoms of traumatic brain damage based on the K. Cicerone questionnaire, and the severity of PTSD based on PCL-military tests. SPECT investigation was carried out using 99mTc-hexamethyl-propylene-amine-oxime (99mTc-HMPAO). The main quantitative criteria for the analysis of SPECT images were volumetric cerebral blood flow (CBF) and intrahemispheric symmetry (IHS) of perfusion in brain segments. Based on the comparison of CBF and IHS in segments of the brain with the NPT data, the highly correlated relationships were obtained that amounted from 0.82 to 0.90. At the same time, for each of NPT tests, 3–4 brain segments could be singled out, where CBF and IHS to the fullest extent reflect the neuro-cognitive state of the patient. It has been shown for the first time that on the basis of objective SPECT data with 99mTc-HMPAO it is possible to quantify the patient’s neuro-cognitive state. The research results can be recommended for a wider use in departments of radionuclide diagnostics when examining the military personnel with TBI in the aftermath of CC.
References
- S. R. Millis et al., “Long-term neuropsychological outcome after traumatic brain injury,” J. Head Trauma Rehabil., vol. 16, no. 4, pp. 343–355, 2001, doi: https://doi.org/10.1097/00001199-200108000-00005.
- J. J. Vasterling et al., “Longitudinal associations among posttraumatic stress disorder symptoms, traumatic brain injury, and neurocognitive functioning in army soldiers deployed to the Iraq war,” J. Int. Neuropsychol. Soc., vol. 24, no. 4, pp. 311–323, 2018, doi: https://doi.org/10.1017/S1355617717001059.
- R. F. Armenta, T. Rush, C. A. LeardMann, J. Millegan, A. Cooper, C. W. Hoge, “Factors associated with persistent posttraumatic stress disorder among U.S. military service members and veterans,” BMC Psychiatry, vol. 18, no. 1, p. 48, 2018, doi: https://doi.org/10.1186/s12888-018-1590-5.
- I. Giesinger, J. Li, E. Takemoto, J. E. Cone, M. R. Farfel, R. M. Brackbill, “Association between posttraumatic stress disorder and mortality among responders and civilians following the September 11, 2001, disaster,” JAMA Netw. Open, vol. 3, no. 2, p. e1920476, 2020, doi: https://doi.org/10.1001/jamanetworkopen.2019.20476.
- A. M. Kelley, B. M. Ranes, A. Estrada, C. M. Grandizio, “Evaluation of the military functional assessment program,” J. Head Trauma Rehabil., vol. 30, no. 4, pp. E11–E20, 2015, doi: https://doi.org/10.1097/HTR.0000000000000060.
- A. M. Kelley, M. Showers, “Evaluation of the military functional assessment program for return-to-duty decision making: A longitudinal study,” Mil. Med., vol. 184, no. Supplement_1, pp. 160–167, 2019, doi: https://doi.org/10.1093/milmed/usy373.
- H. Ibrahim, V. Ertl, C. Catani, A. A. Ismail, F. Neuner, “The validity of posttraumatic stress disorder checklist for DSM-5 (PCL-5) as screening instrument with Kurdish and Arab displaced populations living in the Kurdistan region of Iraq,” BMC Psychiatry, vol. 18, no. 1, p. 259, 2018, doi: https://doi.org/10.1186/s12888-018-1839-z.
- I. A. Frankova, “Current courses for diagnostics and treatment of post-traumatic stress disorder (review),” Psychiatry and Psychopharmacotherapy, vol. 18, no. 1, pp. 52–60, 2016.
- J. Newmark, T. L. Richards, “Delayed unilateral post-traumatic tremor: Localization studies using single-proton computed tomographic and magnetic resonance spectroscopy techniques,” Mil. Med., vol. 164, no. 1, pp. 59–64, 1999, doi: https://doi.org/10.1093/milmed/164.1.59.
- J. D. Lewine et al., “Objective documentation of traumatic brain injury subsequent to mild head trauma,” J. Head Trauma Rehabil., vol. 22, no. 3, pp. 141–155, 2007, doi: https://doi.org/10.1097/01.HTR.0000271115.29954.27.
- N. J. Kolla, S. Houle, “Single-photon emission computed tomography and positron emission tomography studies of antisocial personality disorder and aggression: a targeted review,” Curr. Psychiatry Reports, vol. 21, no. 4, p. 24, 2019, doi: https://doi.org/10.1007/s11920-019-1011-6.
- N. A. Nikolov, S. S. Makeiev, T. G. Novikova, V. O. Tsikalo, Y. S. Kriukova, “Intrahemispheric symmetry of brain perfusion. Part 1. Calculation procedure,” Radioelectron. Commun. Syst., vol. 64, no. 8, pp. 403–412, 2021, doi: https://doi.org/10.3103/S073527272108001X.
- N. A. Nikolov, T. G. Novikova, S. S. Makeiev, V. V. Stebliuk, V. O. Tsikalo, “Intrahemispheric symmetry of brain perfusion. Part 2. Clinical investigations,” Radioelectron. Commun. Syst., vol. 65, no. 5, pp. 235–247, 2022, doi: https://doi.org/10.3103/S0735272722050028.
- H. Haken, Principles of Brain Functioning: A Synergetic Approach to Brain Activity, Behavior and Cognition. Springer, 2012.
- M. I. Rabinovich, M. K. Muezzinoglu, “Nonlinear dynamics of the brain: emotion and cognition,” Uspekhi Fiz. Nauk, vol. 180, no. 4, p. 371, 2010, doi: https://doi.org/10.3367/UFNr.0180.201004b.0371.
- X. Xu, Y. Liu, Z. Zhang, “Study on mutation mechanism of victim’s psychological behavior state after major natural disasters,” J. Risk Anal. Cris. Response, vol. 10, no. 2, p. 27, 2020, doi: https://doi.org/10.2991/jracr.k.200415.001.
- G. A. Fastovtsov, “Determination of the risk of criminal-aggressive behavior among combatants,” Criminalistics, vol. 5, pp. 48–58, 2018, uri: https://millaw.ru/uploads/2018/05/48-58.pdf.
- P. N. C. for PTSD, “PTSD checklist for DSM-5 (PCL-5),” U. S. Department of Veterans Affairs. https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp#obtain.
- K. C. Wilkins, A. J. Lang, S. B. Norman, “Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions,” Depress. Anxiety, vol. 28, no. 7, pp. 596–606, 2011, doi: https://doi.org/10.1002/da.20837.
- A. M. Wayne, Vegetative Disorders - Clinical Picture, Diagnosis, Treatment. Moscow: Neurology, 2001.
- V. I. Tsymbaliuk et al., Okhorona mentalnoho zdorovia ta medyko-psykholohichna reabilitatsiia viiskovosluzhbovtsiv v umovakh hibrydnoi viiny: teoriia i praktyka, [in Ukrainian]. Kyiv: Medytsyna, 2021.
- N. A. Nikolov et al., “Determination of absolute cerebral blood flow scintigraphy with lipophilic radiopharmaceutical,” Med. Phys., no. 3, pp. 36–45, 2018, uri: https://elibrary.ru/item.asp?id=35664229.
- N. Nikolov, S. Makeyev, O. Yaroshenko, T. Novikova, M. Globa, “Quantitative evaluation of the absolute value of the cerebral blood flow according to the scintigraphic studies with 99MTC-HMPAO,” Res. Bull. Natl. Tech. Univ. Ukr. “Kyiv Politech. Institute,” no. 1, pp. 61–68, 2017, doi: https://doi.org/10.20535/1810-0546.2017.1.91646.
- M. O. Nikolov, Y. D. Zalisna, T. G. Novikova, S. S. Makeуev, A. V. Duchenko, “Possibilities of brain SPECT with perfusion radiopharmaceuticals for the quantitative assessment of cognitive changes in patients with hypertensive encephalopathy,” Ukr. J. Radiol. Oncol., vol. 30, no. 1, pp. 42–56, 2022, doi: https://doi.org/10.46879/ukroj.1.2022.42-56.