Intrahemispheric symmetry of brain perfusion. Part 2. Clinical investigations
DOI:
https://doi.org/10.3103/S0735272722050028Abstract
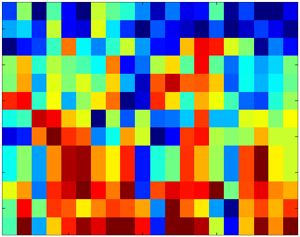
This study presents the assessment of the clinical significance of the quantitative criterion of intrahemispheric symmetry (IHS) of cerebral perfusion according to the data of single-photon emission computed tomography (SPECT) with perfusion radiopharmaceutical in patients with mild cerebral injury due to combat trauma. The results of examination of 44 patients were analyzed. The main materials for comparison included SPECT images of brain with 99mTc-HMPAO and data of the neuropsychological testing (NPT), such as assessment of vegetative disorders according to Wayne, the assessment of psychoemotional sphere, the assessment of the symptom severity of traumatic brain injury based on the Cicerone questionnaire, and the assessment of the severity of post trauma stress disorder (PTSD) based on the PCL-military tests.
The results of the analysis of scatterograms in brain segments for various quantitative NPT criteria and the IHS criterion showed the data clustering and nonlinear relationship. In some cases, this relationship is characterized by threshold effects (catastrophes and bifurcations). Hence, the assessment of psychoemotional and cognitive impairments based on SPECT and IHS data could be expediently carried out on the basis of piecewise polynomial, linear or parabolic functions.
For the first time, the clinical informativeness of the IHS criterion for brain perfusion according to SPECT data has been shown that allows us to assess quantitatively the psychoemotional and cognitive impairments in patients with moderate cerebral injury due to combat contusion accompanied by the development of post trauma stress disorder (PTSD).
References
- A. M. Kelley, M. Showers, “Evaluation of the military functional assessment program for return-to-duty decision making: A longitudinal study,” Mil. Med., vol. 184, no. Supplement_1, pp. 160–167, 2019, doi: https://doi.org/10.1093/milmed/usy373.
- S. M. Keen, “Psychometric properties of PTSD checklist in sample of male veterans,” J. Rehabil. Res. Dev., vol. 45, no. 3, pp. 465–474, 2008, doi: https://doi.org/10.1682/JRRD.2007.09.0138.
- T. Michael, A. Ehlers, S. L. Halligan, D. M. Clark, “Unwanted memories of assault: what intrusion characteristics are associated with PTSD?,” Behav. Res. Ther., vol. 43, no. 5, pp. 613–628, 2005, doi: https://doi.org/10.1016/j.brat.2004.04.006.
- K. Loganovsky, N. Zdanevich, “Psychophysiological peculiarities of post-traumatic stress disorder after the Chernobyl accident,” Int. J. Psychophysiol., vol. 77, no. 3, pp. 340–341, 2010, doi: https://doi.org/10.1016/j.ijpsycho.2010.06.283.
- C. Robba et al., “Brain ultrasonography: methodology, basic and advanced principles and clinical applications. A narrative review,” Intensive Care Med., vol. 45, no. 7, pp. 913–927, 2019, doi: https://doi.org/10.1007/s00134-019-05610-4.
- R. W. Van Boven et al., “Advances in neuroimaging of traumatic brain injury and posttraumatic stress disorder,” J. Rehabil. Res. Dev., vol. 46, no. 6, p. 717, 2009, doi: https://doi.org/10.1682/JRRD.2008.12.0161.
- M. B. Stein et al., “Smaller regional brain volumes predict posttraumatic stress disorder at 3 months after mild traumatic brain injury,” Biol. Psychiatry Cogn. Neurosci. Neuroimaging, vol. 6, no. 3, pp. 352–359, 2021, doi: https://doi.org/10.1016/j.bpsc.2020.10.008.
- Z. Haneef, H. S. Levin, J. D. Frost, E. M. Mizrahi, “Electroencephalography and quantitative electroencephalography in mild traumatic brain injury,” J. Neurotrauma, vol. 30, no. 8, pp. 653–656, 2013, doi: https://doi.org/10.1089/neu.2012.2585.
- P. Miranda, C. D. Cox, M. Alexander, J. R. T. Lakey, S. Danev, “Electroencephalography (EEG)-based detection, management, recovery and brain retraining tracking of Traumatic Brain Injury (TBI) when ‘Only Time Can Tell,’” J. Syst. Integr. Neurosci., vol. 6, no. 3, 2020, doi: https://doi.org/10.15761/JSIN.1000230.
- J. Newmark, T. L. Richards, “Delayed unilateral post-traumatic tremor: Localization studies using single-proton computed tomographic and magnetic resonance spectroscopy techniques,” Mil. Med., vol. 164, no. 1, pp. 59–64, 1999, doi: https://doi.org/10.1093/milmed/164.1.59.
- J. D. Lewine et al., “Objective documentation of traumatic brain injury subsequent to mild head trauma,” J. Head Trauma Rehabil., vol. 22, no. 3, pp. 141–155, 2007, doi: https://doi.org/10.1097/01.HTR.0000271115.29954.27.
- N. A. Nikolov, S. S. Makeiev, T. G. Novikova, V. O. Tsikalo, Y. S. Kriukova, “Intrahemispheric symmetry of brain perfusion. Part 1. Calculation procedure,” Radioelectron. Commun. Syst., vol. 64, no. 8, pp. 403–412, 2021, doi: https://doi.org/10.3103/S073527272108001X.
- K. D. Cicerone, K. Kalmar, “Persistent postconcussion syndrome,” J. Head Trauma Rehabil., vol. 10, no. 3, pp. 1–17, 1995, doi: https://doi.org/10.1097/00001199-199506000-00002.
- G. A. Fastovtsov, “On the identification of the risk of the criminal and aggressive behavior of combatants,” Forensic Sci., vol. 5, pp. 48–58, 2018, uri: https://millaw.ru/uploads/2018/05/48-58.pdf.
- P. N. C. for PTSD, “PTSD checklist for DSM-5 (PCL-5),” U. S. Department of Veterans Affairs. https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp#obtain.
- K. C. Wilkins, A. J. Lang, S. B. Norman, “Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions,” Depress. Anxiety, vol. 28, no. 7, pp. 596–606, 2011, doi: https://doi.org/10.1002/da.20837.
- A. M. Wayne, Vegetative Disorders - Clinical Picture, Diagnosis, Treatment. Moscow: Neurology, 2001.
- N. A. Nikolov et al., “Determination of absolute cerebral blood flow scintigraphy with lipophilic radiopharmaceutical,” Med. Phys., no. 3, pp. 36–45, 2018, uri: https://elibrary.ru/item.asp?id=35664229.
- N. A. Nikolov, Y. D. Zalisna, S. S. Makeyev, P. P. Loshitskiy, B. Y. Kolomiec, A. O. Usenko, “Integral estimate of spatial distribution of 99mTc-HMPAO in brain of patients with mild cognitive changes,” Radioelectron. Commun. Syst., vol. 57, no. 12, pp. 559–565, 2014, doi: https://doi.org/10.3103/S073527271412005X.
- M. Ichise, D. G. Chung, P. Wang, G. Wortzman, B. G. Gray, W. Franks, “Technetium-99m-HMPAO SPECT, CT and MRI in the evaluation of patients with chronic traumatic brain injury: a correlation with neuropsychological performance.,” J. Nucl. Med. Off. Publ. Soc. Nucl. Med., vol. 35, no. 2, pp. 217–26, 1994, uri: http://www.ncbi.nlm.nih.gov/pubmed/8294988.
- S. H. A. Chen, “A study of persistent post-concussion symptoms in mild head trauma using positron emission tomography,” J. Neurol. Neurosurg. Psychiatry, vol. 74, no. 3, pp. 326–332, 2003, doi: https://doi.org/10.1136/jnnp.74.3.326.
- O. Bonne, “Cerebral blood flow in chronic symptomatic mild traumatic brain injury,” Psychiatry Res. Neuroimaging, vol. 124, no. 3, pp. 141–152, 2003, doi: https://doi.org/10.1016/S0925-4927(03)00109-4.
- N. Hattori, K. Ikoma, O. Manabe, K. Kobayashi, T. Shiga, N. Tamaki, “Brain perfusion SPECT demonstrated brain regions responsible for lower processing speed in patients with diffuse traumatic brain injury,” J. Nucl. Med., vol. 55, no. 1, p. 1877, 2014, uri: https://jnm.snmjournals.org/content/55/supplement_1/1877.
- D. Amen, M. Stubblefield, B. Carmichael, R. Thisted, “Brain SPECT findings and aggressiveness,” Ann. Clin. Psychiatry, vol. 8, no. 3, pp. 129–137, 1996, doi: https://doi.org/10.3109/10401239609147750.
- I. Goethals et al., “Cognitive neuroactivation using SPECT and the stroop colored word test in patients with diffuse brain injury,” J. Neurotrauma, vol. 21, no. 8, pp. 1059–1069, 2004, doi: https://doi.org/10.1089/0897715041651051.
- G. Haken, How the Brain Works: A Synergistic Approach to Brain Activity, Behavior, and Cognitive Performance, [in Russian]. Moscow: PER CE, 2001.
- I. Tsuda, “Chaotic itinerancy and its roles in cognitive neurodynamics,” Curr. Opin. Neurobiol., vol. 31, pp. 67–71, 2015, doi: https://doi.org/10.1016/j.conb.2014.08.011.
- R. Rasmussen, M. H. Jensen, M. L. Heltberg, “Chaotic dynamics mediate brain state transitions, driven by changes in extracellular ion concentrations,” Cell Syst., vol. 5, no. 6, pp. 591-603.e4, 2017, doi: https://doi.org/10.1016/j.cels.2017.11.011.
- M. I. Rabinovich, M. K. Muezzinoglu, “Nonlinear dynamics of the brain: emotion and cognition,” Uspekhi Fiz. Nauk, vol. 180, no. 4, p. 371, 2010, doi: https://doi.org/10.3367/UFNr.0180.201004b.0371.