Research of pulse signals mutual influence in polysphygmography of radiary arteries
DOI:
https://doi.org/10.3103/S0735272720080063Keywords:
polysphygmography, mechanical impedance, pulse signals mutual influenceAbstract
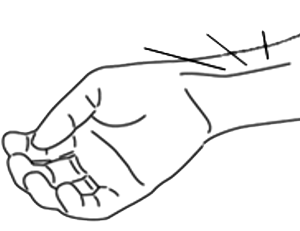
The independence estimation results of synchronously recorded pulse signals in distal parts of human radial arteries are presented in this paper. The study is carried out by the methods of structural-functional and simulation modeling in approximation of an equivalent planar movement of the biological object structural elements. Their elastic characteristics are taken into account using by electromechanical analogies. The correctness of the proposed mathematical model of pulse signals at transducer input is confirmed experimentally. The experimental studies are carried out using a device that represents piezoelectric and piezoresistive transducers connected in series (mechanically). The stiffness and the operating frequency range of the device are equal to 5217 ± 430 N/m and 0.04–32 Hz, respectively. Measurement results for a pulse signal of the piezoelectric transducer (pelot diameters are equal to 6 and 8 mm) and the piezoresistive force sensor show that in the range of transducer to zone surface pressing up to 2 N, the length of arteries areas, forming pulse signals, does not exceed 13 mm and is situated within zones accepted in oriental medicine.References
- D.-Y. Zhang, W.-M. Zuo, D. Zhang, H.-Z. Zhang, N.-M. Li, “Wrist blood flow signal-based computerized pulse diagnosis using spatial and spectrum features,” J. Biomed. Sci. Eng., vol. 03, no. 04, pp. 361–366, 2010, doi: https://doi.org/10.4236/jbise.2010.34050.
- A. A. Fedotov, “Techniques for the morphological analysis of the pulse wave,” Biomed. Eng., vol. 53, no. 4, pp. 270–274, 2019, doi: https://doi.org/10.1007/s10527-019-09924-x.
- A. A. Fedotov, “A pulse wave monitor with adaptive filtering of motion artifacts,” Biomed. Eng., vol. 53, no. 6, pp. 375–379, 2020, doi: https://doi.org/10.1007/s10527-020-09946-w.
- A. A. Desova, V. V. Guchuk, Y. A. Dorofeyuk, A. M. Anokhin, “Procedure for formation of features of the radial artery pulsation signal,” Biomed. Eng., vol. 46, no. 4, pp. 149–153, 2012, doi: https://doi.org/10.1007/s10527-012-9291-8.
- X. Wang, K. Yu, Y. Luo, M. Zhong, “Prospect of the objectification of pulse diagnosis in traditional chinese medicine in the age of big data,” in Proceedings of the 2019 International Conference on Organizational Innovation, 2019, pp. 809–814, doi: https://doi.org/10.2991/icoi-19.2019.143.
- I. S. Yavelov, I. V. Stepanyan, A. V. Rochagov, A. V. Zholobov, R. I. Yavelov, O. I. Yavelov, “Pulse wave sensor sensitivity to changing the point of measurement,” Biomed. Eng., vol. 53, no. 2, pp. 134–136, 2019, doi: https://doi.org/10.1007/s10527-019-09893-1.
- K. Goyal, R. Agarwal, “Pulse based sensor design for wrist pulse signal analysis and health diagnosis,” Biomed. Res., vol. 28, no. 12, pp. 5187–5195, 2017, uri: www.biomedres.info.
- A. Bhinav, M. Sareen, M. Kumar, J. Santhosh, A. Salhan, S. Anand, “Nadi yantra: a robust system design to capture the signals from the radial artery for assessment of the autonomic nervous system non-invasively,” J. Biomed. Sci. Eng., vol. 02, no. 07, pp. 471–479, 2009, doi: https://doi.org/10.4236/jbise.2009.27068.
- E. V. Storchun, V. V. Boronoev, “Specific features of the procedure for synchronous pulse wave detection,” Biomed. Eng., vol. 39, no. 2, pp. 79–81, 2005, doi: https://doi.org/10.1007/s10527-005-0051-x.
- Y. Storchun, A. Klymukh, “Dynamics of pulse signal forming from distal zones of radial arteries,” Bull. Lviv Polytech. Natl. Univ. Ser. Radio Electron. Telecommun., no. 766, pp. 202–207, 2013.
- V. А. Golikov, S. G. Odintsov, “Effect of primary transducers on human body mechanical impedance,” Med. Technol. News, no. 3, pp. 25–28, 1978.
- Y. Luo, S. Niu, J. Cordero, H. Deng, Y. Shen, “Bioinspired non-invasive radial pulse sensor: from biomimetic design, system calibration, to clinic application,” Robot. Biomimetics, vol. 1, no. 1, p. 19, 2014, doi: https://doi.org/10.1186/s40638-014-0019-y.
- N. N. Savitskiy, Biophysical Foundations of Blood Circulation and Clinical Methods for Hemodynamics Studying. Leningrad: Medicine, 1974.
- Е. V. Storchun, V. V. Boronoev, “The study of the pulse signals formation of the radial artery,” ESSUTM Bull., no. 5, pp. 53–58, 2014.
- M. E. Lockhart, M. L. Robbin, M. Allon, “Preoperative sonographic radial artery evaluation and correlation with subsequent radiocephalic fistula outcome,” J. Ultrasound Med., vol. 23, no. 2, pp. 161–168, 2004, doi: https://doi.org/10.7863/jum.2004.23.2.161.
- A. C. Y. Tang, J. W. Y. Chung, T. K. S. Wong, “Validation of a novel traditional chinese medicine pulse diagnostic model using an artificial neural network,” Evidence-Based Complement. Altern. Med., vol. 2012, pp. 1–7, 2012, doi: https://doi.org/10.1155/2012/685094.
Downloads
Published
2020-08-26
Issue
Section
Research Articles