Reconstruction of action potentials of cardiac cells from extracellular field potentials
DOI:
https://doi.org/10.3103/S0735272722090047Abstract
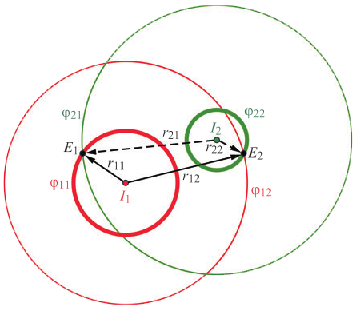
The key areas of application of systems with microelectrode arrays (MEA) are studying the mechanisms of diseases and testing the effect of drugs on the human body using “laboratory-on-a-chip” technologies based on researches of artificially grown cells. Many scientists’ efforts are directed to the processing and analysis of information received by MEA systems, helping the doctors in creating effective treatment strategies. However, field potentials (FP) of cardiac cells recorded with MEA systems in non-invasive measurements provide incomplete information for the estimation of ionic currents, compared to invasive measurements of action potentials (AP) obtained using patch-clamp technology. The research is devoted to the mathematical determination of the relationship between the signals of electrical activity of cardiomyocytes: internal AP and external FP. In this paper it is proposed a method for solving the inverse problem of the relationship between AP and FP. The equation for the transfer functions between AP and FP is obtained on the basis of field theory. The paper presents the results of AP reconstruction modeling using measured FPs, demonstrating the change in the morphology and parameters of these signals under the influence of dimethylsulfoxide (DMSO). FP signals are recorded using non-destructive electrophysiological technology based on microelectrode coaxial guides (mECG), which can be considered as a type of MEA.
References
P. Garg, V. Garg, R. Shrestha, M. C. Sanguinetti, T. J. Kamp, J. C. Wu, “Human induced pluripotent stem cell–derived cardiomyocytes as models for cardiac channelopathies,” Circ. Res., vol. 123, no. 2, pp. 224–243, 2018, doi: https://doi.org/10.1161/CIRCRESAHA.118.311209.
N. Azizipour, R. Avazpour, D. H. Rosenzweig, M. Sawan, A. Ajji, “Evolution of biochip technology: A review from lab-on-a-chip to organ-on-a-chip,” Micromachines, vol. 11, no. 6, p. 599, 2020, doi: https://doi.org/10.3390/mi11060599.
J. Piñero, L. I. Furlong, F. Sanz, “In silico models in drug development: where we are,” Curr. Opin. Pharmacol., vol. 42, pp. 111–121, 2018, doi: https://doi.org/10.1016/j.coph.2018.08.007.
H.-J. Huang, Y.-H. Lee, Y.-H. Hsu, C.-T. Liao, Y.-F. Lin, H.-W. Chiu, “Current strategies in assessment of nanotoxicity: alternatives to in vivo animal testing,” Int. J. Mol. Sci., vol. 22, no. 8, p. 4216, 2021, doi: https://doi.org/10.3390/ijms22084216.
L. D. Garma et al., “Cost-effective and multifunctional acquisition system for in vitro electrophysiological investigations with multi-electrode arrays,” PLOS ONE, vol. 14, no. 3, p. e0214017, 2019, doi: https://doi.org/10.1371/journal.pone.0214017.
L. G. J. Tertoolen, S. R. Braam, B. J. van Meer, R. Passier, C. L. Mummery, “Interpretation of field potentials measured on a multi electrode array in pharmacological toxicity screening on primary and human pluripotent stem cell-derived cardiomyocytes,” Biochem. Biophys. Res. Commun., vol. 497, no. 4, pp. 1135–1141, 2018, doi: https://doi.org/10.1016/j.bbrc.2017.01.151.
M. Talkhabi, N. Aghdami, H. Baharvand, “Human cardiomyocyte generation from pluripotent stem cells: A state-of-art,” Life Sci., vol. 145, pp. 98–113, 2016, doi: https://doi.org/10.1016/j.lfs.2015.12.023.
P. Mulder et al., “Predicting cardiac safety using human induced pluripotent stem cell-derived cardiomyocytes combined with multi-electrode array (MEA) technology: A conference report,” J. Pharmacol. Toxicol. Methods, vol. 91, pp. 36–42, 2018, doi: https://doi.org/10.1016/j.vascn.2018.01.003.
J. Ma et al., “High purity human-induced pluripotent stem cell-derived cardiomyocytes: electrophysiological properties of action potentials and ionic currents,” Am. J. Physiol. Circ. Physiol., vol. 301, no. 5, pp. H2006–H2017, 2011, doi: https://doi.org/10.1152/ajpheart.00694.2011.
A. S. T. Smith, J. Macadangdang, W. Leung, M. A. Laflamme, D.-H. Kim, “Human iPSC-derived cardiomyocytes and tissue engineering strategies for disease modeling and drug screening,” Biotechnol. Adv., vol. 35, no. 1, pp. 77–94, 2017, doi: https://doi.org/10.1016/j.biotechadv.2016.12.002.
P. W. Burridge, G. Keller, J. D. Gold, J. C. Wu, “Production of De Novo Cardiomyocytes: Human pluripotent stem cell differentiation and direct reprogramming,” Cell Stem Cell, vol. 10, no. 1, pp. 16–28, 2012, doi: https://doi.org/10.1016/j.stem.2011.12.013.
S. Casini, A. O. Verkerk, C. A. Remme, “Human iPSC-derived cardiomyocytes for investigation of disease mechanisms and therapeutic strategies in inherited arrhythmia syndromes: Strengths and limitations,” Cardiovasc. Drugs Ther., vol. 31, no. 3, pp. 325–344, 2017, doi: https://doi.org/10.1007/s10557-017-6735-0.
L. A. Annecchino, S. R. Schultz, “Progress in automating patch clamp cellular physiology,” Brain Neurosci. Adv., vol. 2, p. 239821281877656, 2018, doi: https://doi.org/10.1177/2398212818776561.
S. A. Mann et al., “Recording of multiple ion current components and action potentials in human induced pluripotent stem cell-derived cardiomyocytes via automated patch-clamp,” J. Pharmacol. Toxicol. Methods, vol. 100, p. 106599, 2019, doi: https://doi.org/10.1016/j.vascn.2019.106599.
T. J. Herron, P. Lee, J. Jalife, “Optical imaging of voltage and calcium in cardiac cells & tissues,” Circ. Res., vol. 110, no. 4, pp. 609–623, 2012, doi: https://doi.org/10.1161/CIRCRESAHA.111.247494.
M. C. Müllenbroich et al., “Novel optics-based approaches for cardiac electrophysiology: A review,” Front. Physiol., vol. 12, 2021, doi: https://doi.org/10.3389/fphys.2021.769586.
E. Tanumihardja, D. S. de Bruijn, R. H. Slaats, W. Olthuis, A. van den Berg, “Monitoring contractile cardiomyocytes via impedance using multipurpose thin film ruthenium oxide electrodes,” Sensors, vol. 21, no. 4, p. 1433, 2021, doi: https://doi.org/10.3390/s21041433.
M. F. Peters, C. W. Scott, R. Ochalski, Y. P. Dragan, “Evaluation of cellular impedance measures of cardiomyocyte cultures for drug screening applications,” ASSAY Drug Dev. Technol., vol. 10, no. 6, pp. 525–532, 2012, doi: https://doi.org/10.1089/adt.2011.442.
M. F. Peters, S. D. Lamore, L. Guo, C. W. Scott, K. L. Kolaja, “Human stem cell-derived cardiomyocytes in cellular impedance assays: Bringing cardiotoxicity screening to the front line,” Cardiovasc. Toxicol., vol. 15, no. 2, pp. 127–139, 2015, doi: https://doi.org/10.1007/s12012-014-9268-9.
B. Koci et al., “An impedance-based approach using human iPSC-derived cardiomyocytes significantly improves in vitro prediction of in vivo cardiotox liabilities,” Toxicol. Appl. Pharmacol., vol. 329, pp. 121–127, 2017, doi: https://doi.org/10.1016/j.taap.2017.05.023.
C. W. Scott, X. Zhang, N. Abi-Gerges, S. D. Lamore, Y. A. Abassi, M. F. Peters, “An impedance-based cellular assay using human iPSC-derived cardiomyocytes to quantify modulators of cardiac contractility,” Toxicol. Sci., vol. 142, no. 2, pp. 331–338, 2014, doi: https://doi.org/10.1093/toxsci/kfu186.
G. Melle et al., “Intracellular recording of human cardiac action potentials on market-available multielectrode array platforms,” Front. Bioeng. Biotechnol., vol. 8, 2020, doi: https://doi.org/10.3389/fbioe.2020.00066.
M. Dipalo et al., “Plasmonic meta-electrodes allow intracellular recordings at network level on high-density CMOS-multi-electrode arrays,” Nat. Nanotechnol., vol. 13, no. 10, pp. 965–971, 2018, doi: https://doi.org/10.1038/s41565-018-0222-z.
G. C. Messina et al., “Spatially, temporally, and quantitatively controlled delivery of broad range of molecules into selected cells through plasmonic nanotubes,” Adv. Mater., vol. 27, no. 44, pp. 7145–7149, 2015, doi: https://doi.org/10.1002/adma.201503252.
S. R. Braam, L. Tertoolen, A. van de Stolpe, T. Meyer, R. Passier, C. L. Mummery, “Prediction of drug-induced cardiotoxicity using human embryonic stem cell-derived cardiomyocytes,” Stem Cell Res., vol. 4, no. 2, pp. 107–116, 2010, doi: https://doi.org/10.1016/j.scr.2009.11.004.
S. Nachimuthu, M. D. Assar, J. M. Schussler, “Drug-induced QT interval prolongation: mechanisms and clinical management,” Ther. Adv. Drug Saf., vol. 3, no. 5, pp. 241–253, 2012, doi: https://doi.org/10.1177/2042098612454283.
F. Stillitano et al., “Modeling susceptibility to drug-induced long QT with a panel of subject-specific induced pluripotent stem cells,” eLife, vol. 6, 2017, doi: https://doi.org/10.7554/eLife.19406.
N. G. Ivanushkina, K. O. Ivanko, M. O. Shpotak, Y. V. Prokopenko, “Solving the inverse problem of relationship between action potentials and field potentials in cardiac cells,” Visnyk NTUU KPI Seriia - Radiotekhnika Radioaparatobuduvannia, no. 85, pp. 53–59, 2021, doi: https://doi.org/10.20535/RADAP.2021.85.53-59.
R. Visone et al., “Micro-electrode channel guide (µECG) technology: an online method for continuous electrical recording in a human beating heart-on-chip,” Biofabrication, vol. 13, no. 335026, 2021, doi: https://doi.org/10.1088/1758-5090/abe4c4.
A. O. Verkerk et al., “Single cells isolated from human sinoatrial node: Action potentials and numerical reconstruction of pacemaker current,” in 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2007, pp. 904–907, doi: https://doi.org/10.1109/IEMBS.2007.4352437.
C. Rickert, C. Proenza, “ParamAP: Standardized parameterization of sinoatrial node myocyte action potentials,” Biophys. J., vol. 113, no. 4, pp. 765–769, 2017, doi: https://doi.org/10.1016/j.bpj.2017.07.001.
M. Verheijen et al., “DMSO induces drastic changes in human cellular processes and epigenetic landscape in vitro,” Sci. Reports, vol. 9, no. 1, p. 4641, 2019, doi: https://doi.org/10.1038/s41598-019-40660-0.
X. Zhang et al., “Multi-parametric assessment of cardiomyocyte excitation-contraction coupling using impedance and field potential recording: A tool for cardiac safety assessment,” J. Pharmacol. Toxicol. Methods, vol. 81, pp. 201–216, 2016, doi: https://doi.org/10.1016/j.vascn.2016.06.004.
H. Ando et al., “A new paradigm for drug-induced torsadogenic risk assessment using human iPS cell-derived cardiomyocytes,” J. Pharmacol. Toxicol. Methods, vol. 84, pp. 111–127, 2017, doi: https://doi.org/10.1016/j.vascn.2016.12.003.